- Login
- Search
- Contact Us
-
Have a question? Our team is here to help guide you on your automation journey.
-
Explore support plans designed to match your business requirements.
-
How can we help you?
-
- AI
AI Without the Hype From pilot to full deployment, our experts partner with you to ensure real, repeatable results. Get Started
- Automation Anywhere AI
-
- Solutions
Featured Agentic Solutions
Accounts Payable Invoice automation—No setup. No code. Just results. Accounts Payable
Customer Onboarding Scale KYC/AML workflows. Customer Onboarding
Customer Support Keep queues moving, even at peak load. Customer Support
Healthcare RCM Revenue cycle management that runs itself. Healthcare RCM
- Products
Platform Features
- Agentic process automation (APA)
- Robotic Process Automation (RPA)
- View all Products
-
- Resources
Get Community Edition: Start automating instantly with FREE access to full-featured automation with Cloud Community Edition.
Featured
 Named a 2025 Gartner® Magic Quadrant™ Leader for RPA.Recognized as a Leader for the Seventh Year in a Row Download report Download report
Named a 2025 Gartner® Magic Quadrant™ Leader for RPA.Recognized as a Leader for the Seventh Year in a Row Download report Download report- Become an Expert
- Developer Tools
- Get Support
- View all resources
-
- Partners
Find an Automation Anywhere Partner Explore our global network of trusted partners to support your Automation journey Find a Partner Find a Partner
- Find a Partner
- For Partners
-
Blog
Healthcare Payer Processes Ripe for Automation
Share this:
The healthcare industry, although initially slow to embrace technology, is now fully immersed in its digital transformation efforts, according to a new report by The Everest Group.
The global healthcare IT market, valued at $187 billion in 2019, is predicted to grow at a more than 15.6% compound annual growth rate (CAGR) between 2020 and 2026, reaching $535.6 billion in 2026. Driving this growth is the increasing adoption of artificial intelligence (AI), a push to leverage electronic health records, growing government regulatory mandates, and the urgent need to cut costs.
Automation is an exciting area for healthcare industry players — particularly healthcare payers — to invest in. This means taking a closer look at Robotic Process Automation (RPA) to automate business processes.
The figure below shows some of the business processes that healthcare payers currently rely on. Many of these are still done manually and offer attractive opportunities to improve employee productivity, streamline organizational efficiency, and reduce expenses. 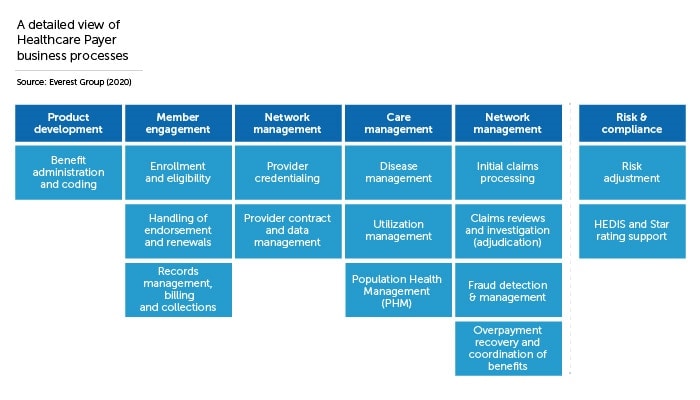
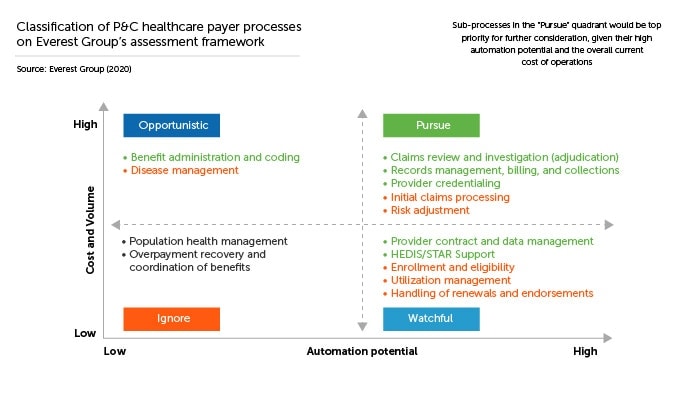
The Everest Group put all these processes through a rigorous evaluation process using a proprietary methodology and divided them into four groups based upon the potential ROI from automating them: pursue them, treat them as opportunistic, be watchful, or ignore them.
In this blog, we will look at one promising process in the “pursue” category, the provider credentialing process, and show you how using intelligent automation — RPA combined with AI — can result in significant time and cost savings.
The four quadrants of automation opportunities
The Everest Group has its way of assessing the suitability of processes for automation. Titled the Enterprise Value Chain Approach (EVCA), this five-step methodology helps businesses identify business processes, define appropriate metrics for successful completion of those processes, analyze each process, spotlight high-value opportunities for automation, and normalize metrics to perform comparisons of and prioritize those opportunities.
The scores divide processes into four quadrants, based on cost-savings potential /volume of transactions and the overall automation potential as follows:
- Pursue: Processes that score high on cost-savings potential/volume of transactions and automation potential fall into this quadrant. These processes are prime candidates to automate immediately.
- Opportunistic: These processes score high on cost savings/transaction volume but low on automation potential. These should be automated on an “opportunistic” basis only — that is when a use case presents itself during the regular course of business operations in which the benefits outweigh the costs.
- Watchful: The processes in this quadrant return relatively little value but are easy to automate. These can be automated when budget/resource capacity allows for it.
- Ignore: These are difficult to automate and return very little value. Ignore them for now.
Provider credentialing: a long, drawn-out process, ready for automation
The healthcare payer value chain is a complex mix of transactional processes with processes that require judgment. Primarily, transactional processes are much more easily automated than those involving human judgment and return a higher ROI. But not all processes are purely transactional or judgment intensive; most are a mixture of both. This is the case with provider credentialing.
Before a provider of healthcare — a physician, for example — can bill an insurance carrier, he or she must first be credentialed. Credentialing is the process by which a healthcare payer — the insurance carrier — formally assesses a provider’s qualifications and competency to join that payer’s provider network. This is an exceedingly time-consuming process that can take months to complete.
The main reason for the length of the process is that physicians need to submit extensive background information — proof of qualifications, skills, training, licenses, as well as answer any questions raised by their backgrounds — some of which are now required to be directly supplied by primary sources such as medical schools and state licensing boards. Asking for and collecting all this data from a variety of disparate sources used to be done manually. Today, RPA enhanced by AI is streamlining this process through intelligent automation.
Attended automation is key to credentialing
The complexity of physical credentialing means that insurance carriers must sometimes incorporate attended RPA when automating it. Attended automation is for situations when it isn’t possible to automate the entire end-to-end process without human intervention. In such cases, the RPA software robot (“bot”) is triggered by a human worker or system-level event and can be thought of as a digital assistant that helps the worker perform better in many ways.
For example, the search for a physician’s state medical license, his or her medical education, board certifications, and potential criminal record all can be automated. Yet, some credential verifications such as obtaining the formal diploma or certificate validation from the medical school and the continuing medical education (CME) credits from accredited institutions still must be completed by a human worker.
Even so, the advantages of automating and accelerating a significant chunk of credentialing can have a big payback for healthcare payers. For starters, it can address the opportunity cost in earnings to the physician and the delay for the payer in adding that physician and his or her patients to its network. Second, manual processing results in a significant number of data entry errors that could be eliminated through automation. And finally, searching for and retrieving data from different sources and reconciling it in a central location is an excellent task for RPA.
The Everest Group identified more than 100 data checks in the physician credentialing process that could be performed by bots automatically before auditing and review by human workers, potentially saving hundreds of hours of labor.
The benefits? Significantly lower costs in credentialing, reduced processing time, and much greater accuracy through eliminating manual data entry errors.
Learn More about the EVCA Approach.
About Automation Anywhere Staff
Get to know the Agentic Process Automation System.

For Students & Developers
Start automating instantly with FREE access to full-featured automation with Cloud Community Edition.



