What do faster claims feel like? See for yourself.
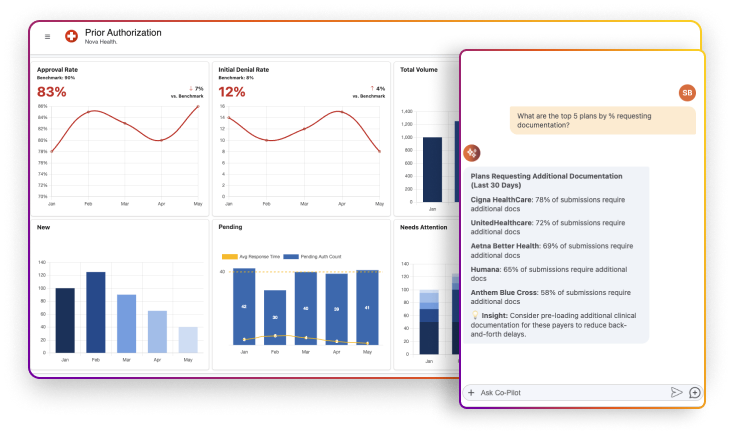
Surface and fix bottlenecks before they slow you down. Our Agentic Solution provides key insights into approval rates, denial patterns, and claim volumes across payers. Ask your agent your most pressing questions and get instant insights with actionable recommendations—like pre-loading clinical docs for problem payers to avoid delays.
Your AI agent helps you stop playing guessing games with payers.
Less chasing, more approvals. Our agentic solution provides all the information you need, from patient details to the complete prior authorization process, with real-time status updates and alerts for what needs attention. Your agent analyzes criteria match scores against approval guidelines and tells you exactly what you should do next.
One click to submit, and your AI agent takes it from there.
From submission to approval without the runaround. Hit submit, and our agentic solution handles everything: submits to the payer, tracks status, flags reviews, and updates your EHR. When clinical documentation is needed, upload it, and your agent resubmits it automatically.
No more phone calls or manual follow-ups—just approvals flowing straight into your system.
Scale RCM performance without adding resources.
Process claims and resubmissions up to 98% faster - AI agents handle portal logins, extract denial codes, and escalate next steps, so teams stay focused on exceptions, not admin.
Cut claim turnaround time up to 76% and keep AR days under 30. AI agents check claims status, trigger next-best actions, and document across EMR and billing systems.
Reduce write-offs by up to 50% and improve both denial and clean claim rates. AI agents flag missing data, rework denied claims, and draft appeal notes—all on their own.
Say hello to faster, more predictable revenue.

For Students & Developers
Start automating instantly with FREE access to full-featured automation with Cloud Community Edition.



